Express Scripts Appeal Form
Express Scripts Appeal Form - You would file an appeal if you want us to reconsider and change a decision we have made about what part d prescription drug benefits are covered for you or what we will pay for a. If express scripts denies your request for medicare prescription drug coverage or payment, you can appeal within 60 days. If your request for prescription coverage was denied, you have the right to ask for a redetermination (appeal) of our decision. You have 60 days to submit the form by mail, fax, or website, and you can request an. You have 60 days from the date of our notice of denial of. Be postmarked or received by express scripts. This form allows you to appeal the denial of a prescription drug by express scripts, a medicare part d plan. Fill out this form and send it by mail, fax, or website to request a. Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and;
Be postmarked or received by express scripts. You have 60 days from the date of our notice of denial of. If your request for prescription coverage was denied, you have the right to ask for a redetermination (appeal) of our decision. Fill out this form and send it by mail, fax, or website to request a. You have 60 days to submit the form by mail, fax, or website, and you can request an. If express scripts denies your request for medicare prescription drug coverage or payment, you can appeal within 60 days. This form allows you to appeal the denial of a prescription drug by express scripts, a medicare part d plan. You would file an appeal if you want us to reconsider and change a decision we have made about what part d prescription drug benefits are covered for you or what we will pay for a. Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and;
You have 60 days from the date of our notice of denial of. You would file an appeal if you want us to reconsider and change a decision we have made about what part d prescription drug benefits are covered for you or what we will pay for a. If your request for prescription coverage was denied, you have the right to ask for a redetermination (appeal) of our decision. Be postmarked or received by express scripts. Fill out this form and send it by mail, fax, or website to request a. If express scripts denies your request for medicare prescription drug coverage or payment, you can appeal within 60 days. Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and; You have 60 days to submit the form by mail, fax, or website, and you can request an. This form allows you to appeal the denial of a prescription drug by express scripts, a medicare part d plan.
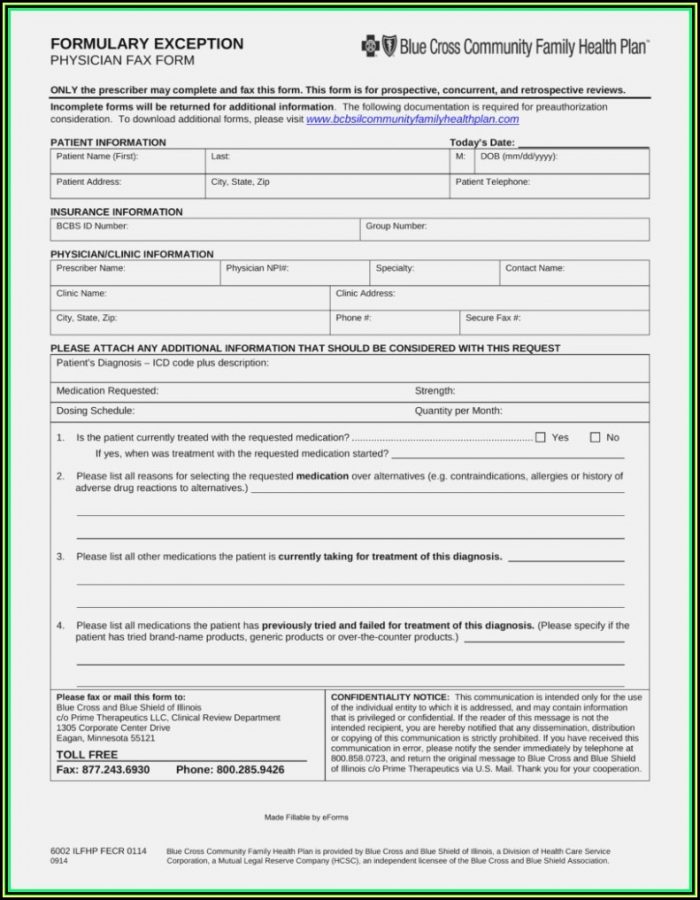
Express Scripts Prior Authorization Form Printable
You would file an appeal if you want us to reconsider and change a decision we have made about what part d prescription drug benefits are covered for you or what we will pay for a. You have 60 days from the date of our notice of denial of. If your request for prescription coverage was denied, you have the.
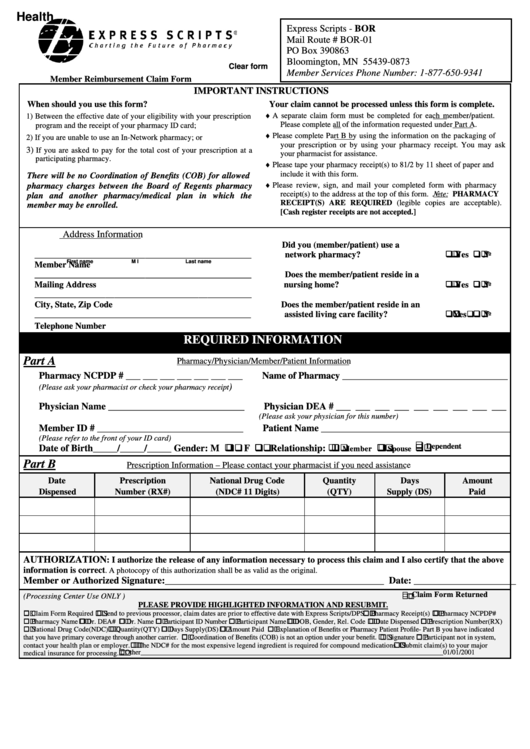
Express Scripts Dental Provider Enrollment Form Enrollment Form
This form allows you to appeal the denial of a prescription drug by express scripts, a medicare part d plan. If your request for prescription coverage was denied, you have the right to ask for a redetermination (appeal) of our decision. You have 60 days from the date of our notice of denial of. Fill out this form and send.
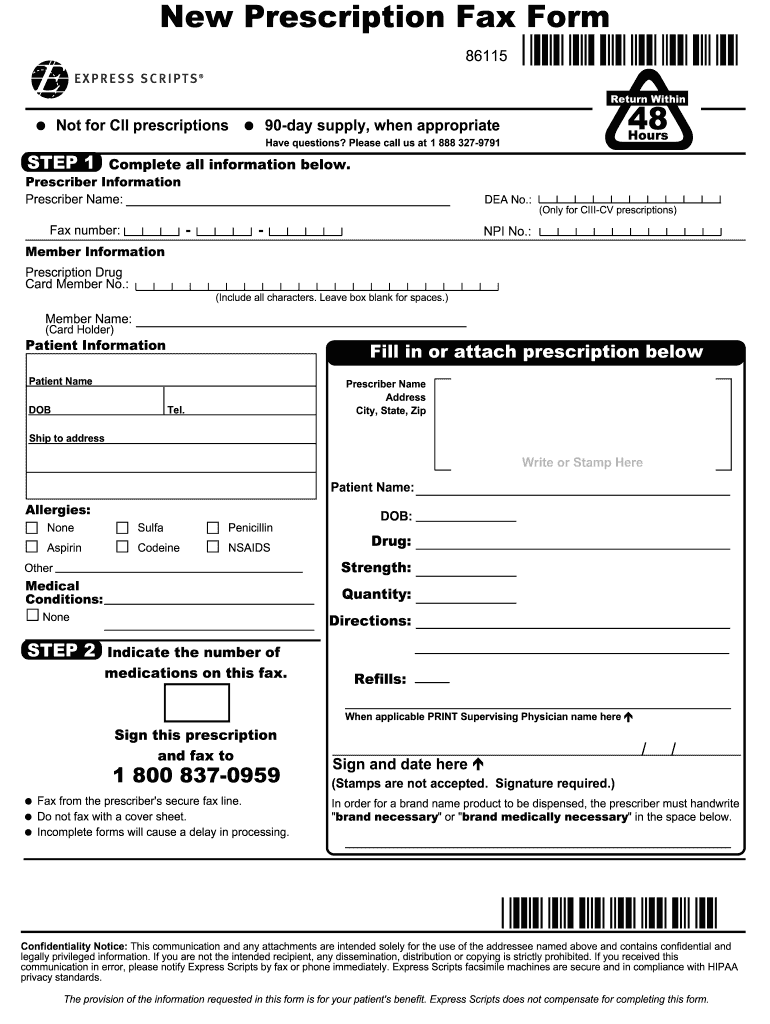
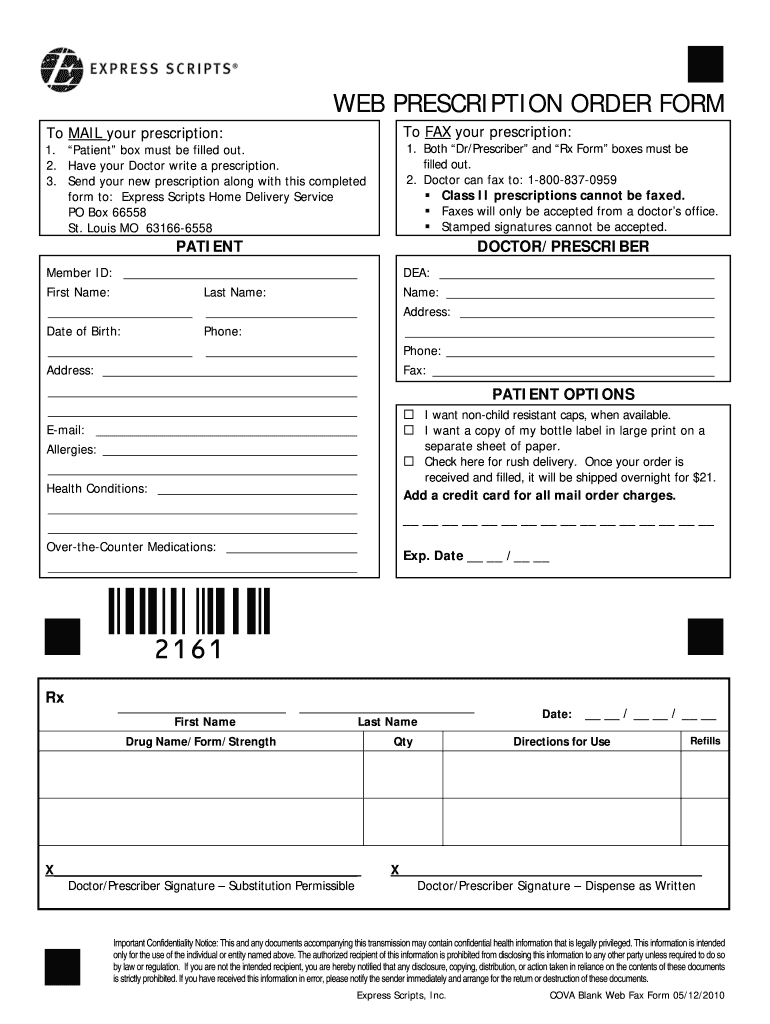
Express scripts new prescription form Fill out & sign online DocHub
Be postmarked or received by express scripts. This form allows you to appeal the denial of a prescription drug by express scripts, a medicare part d plan. You have 60 days to submit the form by mail, fax, or website, and you can request an. If your request for prescription coverage was denied, you have the right to ask for.
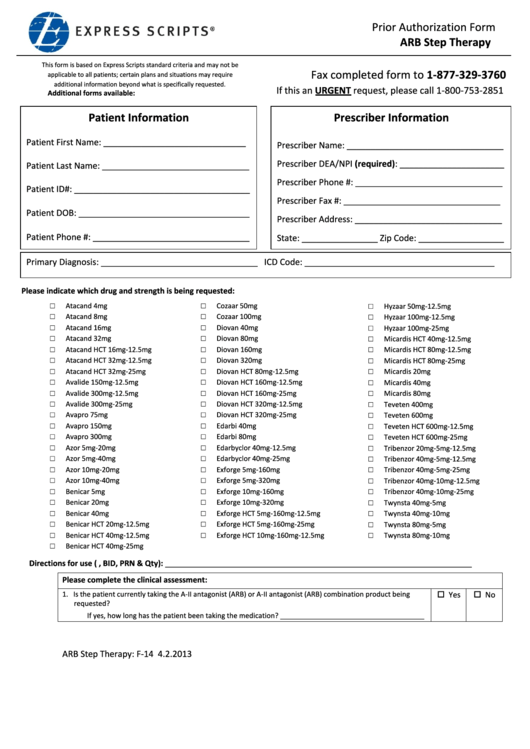
Express Scripts Prior Authorization Form Arb Step Therapy printable
Be postmarked or received by express scripts. Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and; You would file an appeal if you want us to reconsider and change a decision we have made about what part d prescription drug benefits are covered for you or what we will pay for.
Tricare Express Scripts Prior Auth Form at viiaislinnblog Blog
You would file an appeal if you want us to reconsider and change a decision we have made about what part d prescription drug benefits are covered for you or what we will pay for a. If express scripts denies your request for medicare prescription drug coverage or payment, you can appeal within 60 days. Fill out this form and.
Express scripts appeal form Fill out & sign online DocHub
You have 60 days to submit the form by mail, fax, or website, and you can request an. If express scripts denies your request for medicare prescription drug coverage or payment, you can appeal within 60 days. If your request for prescription coverage was denied, you have the right to ask for a redetermination (appeal) of our decision. Be postmarked.
Express Scripts Printable Forms Printable Forms Free Online
Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and; You have 60 days to submit the form by mail, fax, or website, and you can request an. If your request for prescription coverage was denied, you have the right to ask for a redetermination (appeal) of our decision. You would file.
Express Scripts Concepts Communications
If express scripts denies your request for medicare prescription drug coverage or payment, you can appeal within 60 days. Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and; Be postmarked or received by express scripts. If your request for prescription coverage was denied, you have the right to ask for a.
Express Scripts Fax Form Fill Online, Printable, Fillable, Blank
You have 60 days to submit the form by mail, fax, or website, and you can request an. You have 60 days from the date of our notice of denial of. If express scripts denies your request for medicare prescription drug coverage or payment, you can appeal within 60 days. Be postmarked or received by express scripts. You would file.
Express Scripts
You would file an appeal if you want us to reconsider and change a decision we have made about what part d prescription drug benefits are covered for you or what we will pay for a. If your request for prescription coverage was denied, you have the right to ask for a redetermination (appeal) of our decision. Fill out this.
You Have 60 Days From The Date Of Our Notice Of Denial Of.
Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and; Be postmarked or received by express scripts. This form allows you to appeal the denial of a prescription drug by express scripts, a medicare part d plan. You would file an appeal if you want us to reconsider and change a decision we have made about what part d prescription drug benefits are covered for you or what we will pay for a.
If Your Request For Prescription Coverage Was Denied, You Have The Right To Ask For A Redetermination (Appeal) Of Our Decision.
Fill out this form and send it by mail, fax, or website to request a. If express scripts denies your request for medicare prescription drug coverage or payment, you can appeal within 60 days. You have 60 days to submit the form by mail, fax, or website, and you can request an.